This episode of The Dog Show features Dr. John Morgan. John is a Partner Veterinarian at Gordon Vet Hospital, an independently owned vet practice that has been operating since 1971.
After developing an interest in animals at a young age, John studied veterinary science at Sydney University before eventually finding a home at Gordon Vet Hospital where he specialises in orthopaedic conditions and arthritis.
In my second interview with John, we discuss orthopaedic conditions and arthritis in dogs, including breed-specific advice, warning signs for owners, and treatment.
Find out more about Gordon Vet Hospital here:
Listen
Watch
Read
Will: This episode of “The Dog Show” features Dr. John Morgan. John is a partner veterinarian at Gordon Vet Hospital, an independently owned vet practice that has been operating since 1971. After developing an interest in animals at a young age, John studied veterinary science at Sydney University before eventually finding a home at Gordon Vet Hospital, where he specializes in orthopedic conditions and arthritis. In my second interview with John, we discuss orthopedic conditions and arthritis in dogs, including breed-specific advice, warning signs for owners, and treatment. John, welcome back to “The Dog Show” again. It’s good to have you on.
Dr. Morgan: Thanks so much for having me. Good to be here.
Will: Yeah. So today we’re going to talk about orthopedic conditions in dogs and arthritis. It’s one of your specialties. You’ve got a lot of experience in that space. I just want you to give me a quick overview of what that is.
Dr. Morgan: Yeah. So, I guess, it’s a really big range, obviously. When we talk about orthopedic conditions, we talk about, I guess, the malfunction of bones or joints. That’s probably the easiest way to explain it. But that can have an impact on the soft tissues of the muscles and tendons and ligaments surrounding that. So, it is a really, really big field and one that I’m really only scratching the surface of. But it’s, sort of, where I’ve really found my flow as a veterinarian, something that I really enjoy doing that.
Will: So, can you give me some examples of, like, a condition that people might be familiar with or a couple?
Dr. Morgan: Yeah. So, I guess, the most common hindleg condition that we see is what is colloquially known as cruciate ligament disease, so equivalent to an ACL injury. And that basically is a problem that arises with the ligament, the ACL ligament within the joint. It results in instability. And then that instability causes what’s known as arthritis or essentially inflammation of the joint.
Will: Right. So, there’s some sort of shock initially, like an injury, which then results in arthritis. Is that always the case with arthritis?
Dr. Morgan: Not at all. Yeah. No, really good question. So, it is, again, not only multifactorial but it’s sort of a cause…there’s a cause and effect relationship. So, we do see that some dogs actually have an underlying inflammation, which can actually damage that ligament. So, there often isn’t an actual traumatic injury. In most cases, it’s actually just the dog went for a walk or ran a bit too hard at the park, and then, unfortunately, that ligaments gone. But when we look into it there’s actually, again, genetics or potentially alignment issues of that joint that’s caused the problem initially that’s, sort of, not been causing, necessarily, symptoms, but it has been present.
Will: So it sounds like you can, kind of, see some of that early on in a dog’s life, like, there’s warning signs.
Dr. Morgan: There’s warning signs, for sure. And, I mean, probably the one that we try and catch onto earliest, in terms of orthopedic conditions, would be hip dysplasia. So, hip dysplasia or hip instability, as it’s commonly referred to, is actually present from birth in a lot of dogs. They have joints that are extremely loose and they can actually pop in and out of place very easily, and that over time results in arthritis that doesn’t necessarily rear its head until the dog is sort of seven or eight. But there are a lot of warning signs from a very young age that we can pick up or detect on x-rays from very, very young.
Will: Okay. So, with hip dysplasia, you did mention in a previous episode, actually, that labradors are very exposed. Are there other breeds that are more exposed to those and maybe the cruciate ligament ones as well?
Dr. Morgan: Yeah. So, cruciate ligaments are really…it’s probably more to do with lifestyle and weight essentially. So, obviously, cruciate ligament disease will carry in heavier dogs. And there are some breeds, such as in the labrador, unfortunately, are just a bit more prime to cruciate ligament disease. But, yeah, all of the dogs that we see with cruciate ligament disease come from a wide range of different breeds. As for hip dysplasia, there are some really, really standout breeds that are affected, German shepherds, labradors, you know, larger breeds like Newfoundlands. They are all very susceptible to hip dysplasia. Again, it’s a very multifactorial disease. So, their growth rates and their hips seem to predispose them.
Will: Okay. And does that have anything to do with their size, because they are bigger dogs?
Dr. Morgan: Yeah. As far as we can tell, it looks like it is having to do with growth rates. And, again, that, sort of, genetic bottlenecking that we were talking about in a previous episode, that can definitely be a cause and factor, and we do find that genetic heritability is a big feature.
Will: I hear that.
Dr. Morgan: There’s probably been a couple of dogs that have this condition very early on when break is started, and, unfortunately, that’s led to a lot of issues within a lot of dogs.
Will: One condition I’m familiar with because I’ve got a French bulldog, is patella alta. Is that what it’s called?
Dr. Morgan: Patella luxation.
Will: Patella luxation. Yeah, yeah, yeah.
Dr. Morgan: Yeah. So, that’s another…
Will: Is that also an orthopedic condition?
Dr. Morgan: That would be considered [inaudible 00:05:27] orthopedic condition. It’s extremely common in French bulldogs and smaller breed dogs. And we are, obviously…with the training cavoodles, we’re seeing a lot of patella luxation.
Will: That’s why they don’t cover it in insurance.
Dr. Morgan: Yeah. Yeah. The insurance companies are pretty clever about looking at those pre-existing conditions.
Will: Yeah.
Dr. Morgan: But, yes. So, that, again, has a number of different potential causes. It can be traumatic, but in most cases, it is a genetic issue. So, most dogs that we see are, sort of, born with it in varying degrees, and then it can, again, lead to arthritis later in life.
Will: So, I guess, it’s probably hard to do like a catch-all warning sign to look out for for a dog owner, but from an orthopedic, like, let’s say the main ones. Your hip dysplasias, your cruciate ligaments, what should I be looking at for as a new dog owner?
Dr. Morgan: Yeah. So, I guess the ones that we look at, again, being a young-dog disease and what you should be looking for. A sign with the front legs is definitely elbow dysplasia. So, again, if you have a larger breed dog or a dog that has twisted in legs, such as a French bulldog or some Jack Russells, any fallen lameness or front leg lameness in dogs less than six months, would be [inaudible 00:06:36] as soon as we see any sign of pain or any limping after rest. That’s something you need to talk about.
Will: Is that what you meant by lameness? Like limping and…
Dr. Morgan: Yes. So lameness, sorry, is a jargon term. It just refers to any evidence of pain or any dysfunction within the leg. So it’s largely…I may go back to the term lameness, which I’m sorry.
Will: No, it’s all right. Well, now we’ve covered it. You can go back to it as much as you want.
Dr. Morgan: Yeah. We generally use lameness as just basically any sign of pain or injury there.
Will: Okay. Okay.
Dr. Morgan: So, yeah. So, once we identify pain in the elbows, again, we might be suspicious of another condition called elbow dysplasia. With the back legs, often, it’s as simple as an abnormal gait. So, sometimes dogs with luxating patellas or slipping kneecaps, they’ll hold their legs straight back. They’ll, sort of, skip a step occasionally, or when they’re running, they’ll be very suddenly lame or very suddenly they’ll hold a leg up, which is when that pops out of place, which is something you may have noticed as well.
Will: Yeah. Actually, when Frankie was younger that happened quite regularly. When I say regularly, every other walk that she’d like…her whole leg would pop out. She would stop walking. And you’re like, “Oh, my God, what’s happened?” It’s so much like she’s been shot. But I think we discussed it at the time and there were some discussions about we may need knee surgery or looking into different things. But it, kind of, stopped happening and it hasn’t happened for a number of years now, but I’m always alert to it and waiting for [inaudible 00:08:03].
Dr. Morgan: Yeah. And, again, a lot of these conditions, it’s nice to be aware of, but surgery isn’t always the answer. And, certainly, in that case, we would discuss it as an option if it was popping in and out all the time. But, you know, we do, especially these days, we’re very savvy about the risks and benefits associated with surgery. So, we’re not going to recommend surgery. So, they’re not going to be useful or may cause more injury than good.
Will: Well, we’ve got another episode lined up about surgery anyway, so we can talk about that on that one.
Dr. Morgan: Beautiful.
Will: Okay. So, let’s have a look at the common orthopedic conditions you spoke about, cruciate ligament and hip dysplasia, elbow dysplasia. What’s a typical treatment for a dog that has that?
Dr. Morgan: Yeah. So, fortunately, we are catching up a little bit in some of the preventative steps for these procedures. So, starting with hip dysplasia, we do have some early surgical procedures that we can talk about later. As per cruciate ligament disease, early surgical intervention can be useful. In terms of more medical management, it often does rely on, potentially, some injections called pentosan polysulfate, which is basically a nutraceutical drug that helps reduce the inflammation within the joints and improve blood flow. But a lot of these dogs, unfortunately, do require anti-inflammatory drugs more long-term, which is something to reduce inflammation within those joints and to improve quality of life, and to reduce pain associated with arthritis.
Will: Okay. So, I guess, the main thing is more so increasing quality of life. That’s the main treatment, is it?
Dr. Morgan: That’s the main one, especially, you know, once we get past a certain age and arthritis does become more of a problem. Certainly, my focus is on improving quality of life and making sure that they are able to do what they need to do to not only survive but enjoy their lives as well.
Will: So, should owners be walking dogs less or giving them less activity if they do have these? You know, it is a catch-22 because then they put weight on.
Dr. Morgan: Yeah. Yeah. So, definitely, I mean, I’m more of keep them active where I can. There are certain conditions where, you know, obviously, really strenuous exercise like ball chasing or short and fast running around, so dog parks, that kind of thing, they can definitely make things a lot worse. So, obviously, that’s something you probably want to talk about with your vet in certain situations. But, yeah. I’m more for as long as you can, sort of, low-intensity exercise, always on leash just to make sure that they are using their joints, and that can actually help reduce inflammation in the long term.
Will: Okay. So, I guess the walking is good, but the sprinting isn’t so good.
Dr. Morgan: In a lot of cases, yes. That said, obviously, the targets of modern veterinary medicine and surgery these days is actually to get dogs back to that level of activity. So, consult with your vet, obviously. If you’ve got a really active dog, sometimes surgical or medical treatment could get them back to that point, but each case is a little bit different.
Will: Do you notice…I mean, it’s probably hard, there’s not a lot of data on this. But, say, for example, a labrador owner that does those things prior to having the conditions or…as in avoids the excessive exercise, is that going to help not get the conditions?
Dr. Morgan: Well, yeah. Again, another Catch-22 on that one. So, I do find, probably, your classic presentation of the cruciate ligament disease is a, you know, maybe a five or six-year-old quite overweight labrador who hasn’t…unfortunately, their owners haven’t quite had the time to get them out and exercise enough. And what happens is when you don’t use those joints, a lot of the features start to atrophy or shrink or become a lot weaker. So, these dogs will go to the beach or have a rip-roaring weekend at the dog park and that’s when we find those ligaments potentially popping. So they haven’t had that lead-up exercise, similar to us, they haven’t had that sort of training. They haven’t had that regular exercise that reduces the risk of these injuries.
Will: It’s like, someone who hasn’t exercised for like 10 years, they go for a run and they pop their calf.
Dr. Morgan: Pop their calf [inaudible 00:11:53] gone.
Will: Yeah, yeah, yeah.
Dr. Morgan: So, very much the same. Obviously, a lot of what we do is transposed from human physiotherapy and human medicine. But that’s the big one. It’s definitely the under-exercise and then a day at the dog park and they’ve just done too much.
Will: For example, if a pup came in or a young dog came in and you did notice early signs of hip dysplasia or these other conditions, would you recommend a lot of activity scheduled for that dog or would…?
Dr. Morgan: Yeah. It’s a bit of a balance. So, first of all, my suggestion is always getting diagnosis. But, yeah, beyond that, if we see signs of early hip dysplasia, we will talk about reducing what they’re doing and always keeping the weight down. So, weight is definitely one of the leading contributors to hip dysplasia. Basically, that means even if they have hip dysplasia if you keep them lame and you keep them relatively well-exercised, you can reduce the risks. But there are a lot of cases where confining them and leading to more weight loss makes things worse. So, it’s about finding that balance on each dog.
Will: What’s your process for weight management then with dogs? What do you recommend?
Dr. Morgan: Yeah.
Will: This is a broad question.
Dr. Morgan: It’s a broad question and in the consult room it’s very much forthwith. I guess the biggest suggestion is…they’re almost always not as big as us. So, they don’t need the meals that we’re eating. I think a lot of people, sort of, they see the amount of dry food that we’re recommending, and they think, “That’s not gonna fill me. It’s not gonna go fill my dog.” So that sort of considering the size of the pet before you put the meals together and also just measuring it. Me, in particular, over the last few years I’ve had muesli and yogurt and a bit of fruit for breakfast in the morning. That part gets bigger and bigger. I have to stop [inaudible 00:13:40], “Well, I don’t need as much food anymore. I’m just going to shrink it down a little bit.”
Will: Yeah. Portion control is always a great way to lose weight.
Dr. Morgan: Exactly. It works for us and it works for them. And, you know, obviously, the big thing you’re talking about here is exercise for weight loss. As per a lot of human studies and then from what I’ve experienced, you know, they talk about 80% diet and 20% exercise. And the same couldn’t be truer for dogs for sure. You know, we really want to focus on food control or dietary management over just pushing up the exercise, which doesn’t contribute.
Will: Makes a lot of sense. I mean, I’m sure everyone’s had that experience where they’re just smacking themself with exercise and not seeing great results from…
Dr. Morgan: Exactly. Because [inaudible 00:14:22].
Will: Yes.
Dr. Morgan: And you think that’s an excuse to eat well, but, you know, you find that it’ll catch up eventually.
Will: Yeah. You’ve got to balance it out.
Dr. Morgan: Exactly.
Will: So you mentioned the size of the dogs. I mean, it’s common, I guess, if you ever feed your dog off your plate, which you probably don’t recommend anyway, I mean, like, you might think, “Well, something like that, it’s not too big. I’ll just give it to the dog.” That’s, you know, proportionally is massive.
Dr. Morgan: Yeah. We’ve got our test patient, Frankie, here. One small piece of cheese is almost the equivalent of, sort of, a hamburger.
Will: Interesting. Well, we give her a pill every night with a little bit of cheese because that’s the way she likes our [inaudible 00:14:58].
Dr. Morgan: That’s often, you know, a bit of lead-in for it. We think that those little bits of food aren’t going to add much, but again appropriate perspective. So, when we start adding in those table treats, I often do actually recommend reducing what they get in terms of their actual diet. So, taking out of their diet to add to their discretionary foods.
Will: Yeah. So, a trend that I’ve seen a lot, it’s happening out in the states and I guess it’s starting to come in here, is kind of that home delivery food or home-cooked meals for dogs. Is that something you’re seeing as well?
Dr. Morgan: Yeah. Yeah. The raw diets are definitely becoming quite a lot more popular over the, sort of, the commercial dry biscuits. And, I think, that there is definitely a place for them. And I can appreciate why people do like them. I guess it’s always about, you know, talking to your vet about the risk of parasites in raw foods and certainly making sure they are not just home done raw foods. There are a lot of micronutrients that are in pet foods that we may be neglecting. While the dietary requirements are close to ours, they are not exactly the same.
Will: Yeah. So, that’s the raw diet I guess. I can imagine it’s challenging to look after all that food. I mean, you’ve probably got to freeze it or something, do you?
Dr. Morgan: You do. Yeah. I mean, we’ve, sort of, looked at selling the same product, but we’ve obviously got to look at a freezer or, you know, a fridge to have that on offer.
Will: Because there’s also the, kind of, fresh-cooked meals as well, which aren’t raw so much, but they’re meant to be, you know, high nutrients and human-grade.
Dr. Morgan: Yeah. So, I guess, again, it’s the… [inaudible 00:16:34] humans is definitely, traditionally dogs would eat table scraps and there wasn’t a commercial product available. But, again, we’re a little more savvy about nutritional deficiencies that may be coming from that. I think, again, always talk to an expert in the area. So, your local vet will have some tips or just, again, use it as part of the diet. I’m not opposed to using, you know, part dry food and then part of the home-cooked meal option as well.
Will: Okay. So, I guess, if I was to summarize our chat on orthopedic conditions, even though we got a bit sidetracked, weight management, activity, and just having regular checkups with your vet, especially at the young age to just make sure you are on that right path trying to look after it and seeing any early warning signs.
Dr. Morgan: Yeah, 100%. The early warning sign is what we look at. But, yeah, all of those things and obviously looking into their pain management to make sure they’re comfortable.
Will: Cool. Great Thanks, John. Thanks for coming on today.
Dr. Morgan: Will, thanks for having me.
From Our Store
-
French Bulldog Coffee Table Book – The Book of Frenchies
From: AUD $59.99 Add to cart -
Dachshund Coffee Table Book – The Book of Dachshunds
From: AUD $59.99 Add to cart -
Pug Coffee Table Book – The Book of Pugs
AUD $59.99 Add to cart -
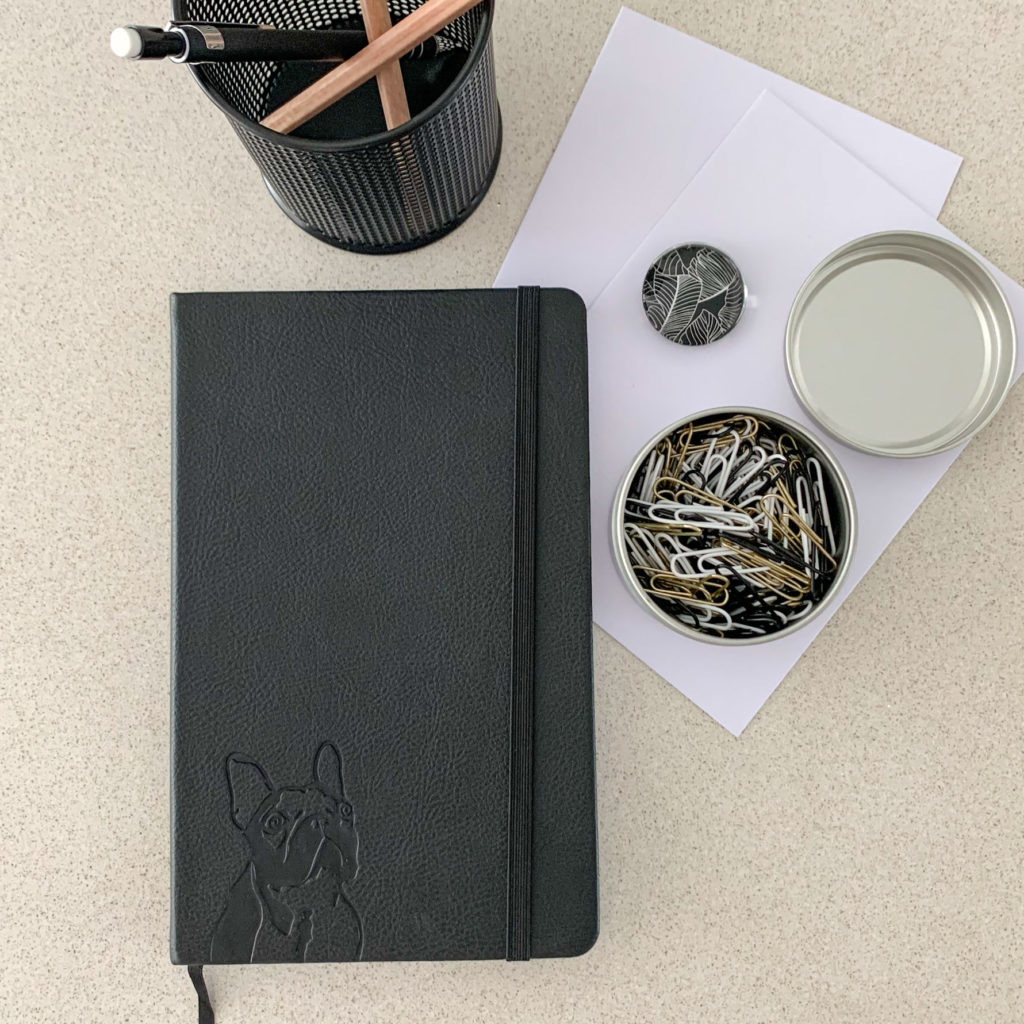
French Bulldog Notebook – A5, Hardcover, PU Leather, 100gsm Lined Pages, Bookmark (Three Colours)
AUD $34.99 Select options -
Dachshund Notebook – A5, Hardcover, PU Leather, 100gsm Lined Pages, Bookmark (Three Colours)
AUD $34.99 Select options -
French Bulldog Planner – PU Leather Exterior, Metal Loose Leaf Ring Binder, 100gsm Paper (Two Colours)
AUD $64.99 Select options -
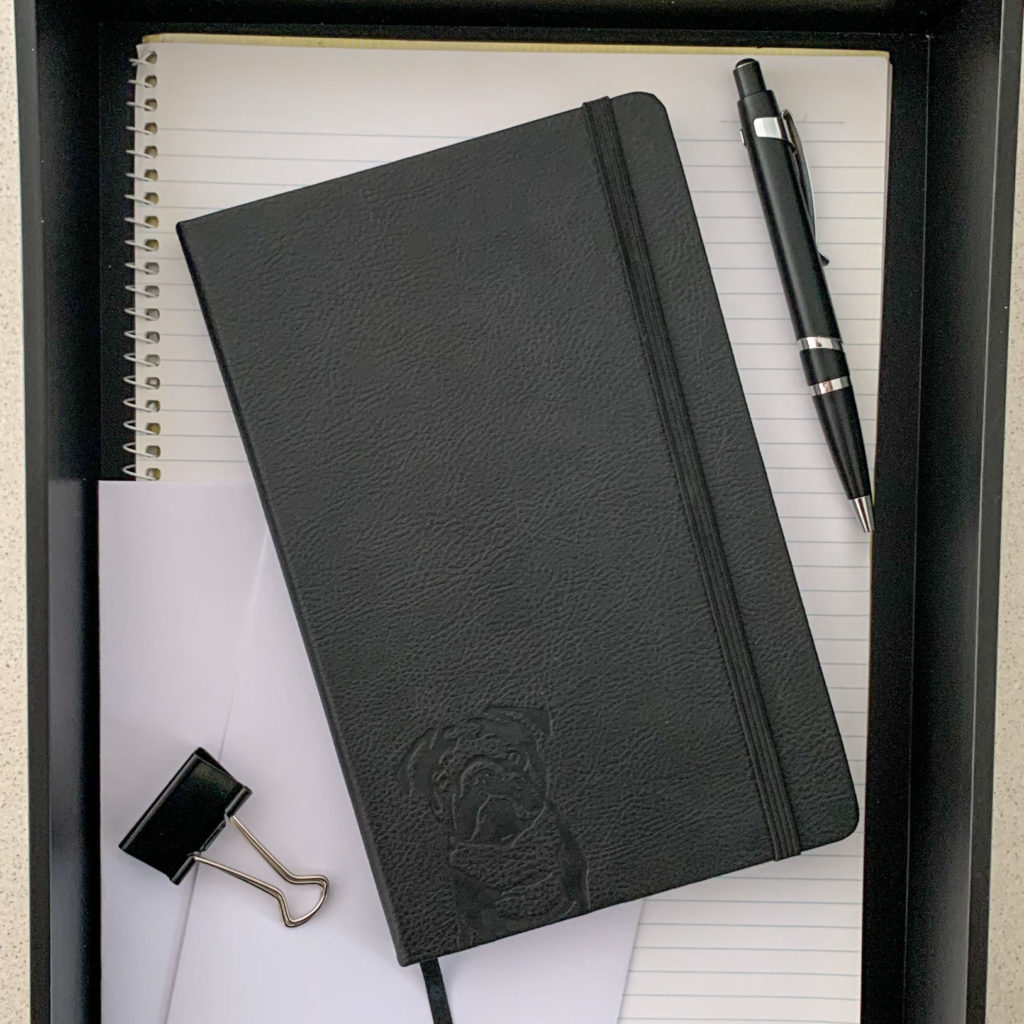
Pug Notebook – A5, Hardcover, Black PU Leather, 100gsm Lined Pages, Bookmark (Three Colours)
AUD $34.99 Select options -
Corgi Notebook – A5, Hardcover, Black PU Leather, 100gsm Lined Pages, Bookmark (Three Colours)
AUD $34.99 Select options -
Dachshund Planner – PU Leather Exterior, Metal Loose Leaf Ring Binder, 100gsm Paper (Two Colours)
AUD $64.99 Select options -
Vizsla/Weimaraner Notebook – A5, Hardcover, PU Leather, 100gsm Lined Pages, Bookmark (Three Colours)
AUD $34.99 Select options -
Cavoodle Notebook – A5, Hardcover, Black PU Leather, 100gsm Lined Pages, Bookmark (Three Colours)
AUD $34.99 Select options -
Beagle Notebook – A5, Hardcover, PU Leather, 100gsm Lined Pages, Bookmark (Three Colours)
AUD $34.99 Select options